Activating people to manage their health and care
A 'one-size-fits-all' approach to healthcare often falls short because it overlooks peoples' unique needs, and their varying levels of activation.
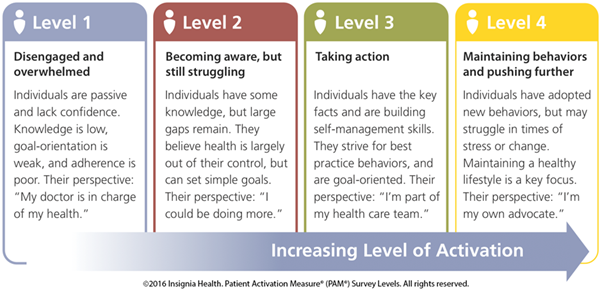
By 'activation' we mean a person's level of knowledge, skills, and confidence to manage their own health.
If care is introduced in a 'one-size-fits-all', non-personalised way, it can lead to those who already have the knowledge, skill, and confidence to manage their health being offered support they don't actually need.
At the other end of the spectrum, it can result in less activated people - those most in need of help - not receiving the support they need. As a result, they may become disengaged, which can ultimately lead to poorer health outcomes for them.
Patient Activation Measures as a solution
The Patient Activation Measure, or PAM, is a tool that provides a structured way to measure and address the diversity of a person's needs, moving away from a generic approach and towards a more personalised and effective model of care.
The PAM helps identify just how 'activated' - knowledgable, capable and confident to manage their health - a person is, which enables healthcare providers to tailor support and interventions accordingly, leading to better patient engagement and outcomes.
WATCH THE VIDEO below to hear Dr Ollie Hart talk about 'Activation' - what it is and how to measure it.

The benefits of the PAM approach
Here's a more detailed look at the benefits of the PAM approach:
Improved Health Outcomes:
- The PAM approach can help improve patient outcomes by fostering self-management behaviors and healthier lifestyle choices, reducing unnecessary emergency department visits, hospital admissions, and readmissions.
Reduced healthcare costs:
- As activated people / patients are more likely to effectively self-manage long-term conditions, and have reduced need for interventions and visits, this naturally leads to a reduction in healthcare costs.
Enhanced patient experience:
- PAM helps tailor healthcare support to a person's individual needs, making them feel more engaged and heard.
- A more collaborative person-provider relationship can improve both the person's and the provider's overall satisfaction with the care delivered.
Other benefits:
- PAM can be used to evaluate the effectiveness of interventions designed to improve patient activation and self-management.
- It can also help identify areas where patients may need additional support and resources.
- By making patient activation central to healthcare delivery, systems can focus on building healthier communities.

How do we decide how activated a person is?
There are a range of tools available that can show how activated a person is.
Have a read through the information below and see where you think your knowledge, support, and readiness are.
You can then try some of the tools to help you have an activation conversation.
Please get in touch and let us know how you get on!
You can even measure it!
There are Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT) codes and templates set up on most clinical systems that allow us to input and then review a person's activation level. That means that we can see progress over time and provide more insight during future periods of care.
What does more activated look and feel like? Does low activation explain anything?
Throughout this work, we have tried to understand what levels of knowledge, support and readiness people have to improve their activation level. We have met people that have lots of knowledge but little support and others who are ready but don’t know where to begin. We’ve also talked to the workforce and heard things like this:
“I’m trying to get them on a PIFU but they’re not listening.”
- Example of agenda driven conversation. Perhaps this person knows what they want and it’s not what is being offered? Perhaps this person is totally overwhelmed by the language you are using?
“How do I end this conversation?”
- Example of someone needing to move on. They’re stuck and don't want to continue. They have other things to be doing, distractions.
“They’ve booked an appointment, but they’ve not attended.”
- Did this person have the knowledge of why they had the appointment? Was it booked with them or for them? Did they get offered it or told they’re having it? There are many reasons why people don’t turn up. Sometimes they are overwhelmed by the experience.
So, how can you tell when someone has high activation?
A conversation tells you a lot about a person but sometimes you learn a lot by observing. Think about the last conversation you had with someone. What did their eye contact and body language tell you?
Common signs of high activation:
- How much time did they talk versus you?
- Did they come prepared with questions for you?
- Was their medication list there, ready to discuss with you?
- Was it obvious that they already had some information about the appointment?
Common signs of low activation:
- Only answer with a yes or no
- Forget or don’t know why they are there
- Slouch and/or avoid eye contact
- Huff / sigh when they sit down to talk to you
- Are agitated or fidgeting
People often bring a chaperone to an appointment. For some, this is a sign that they need help and support with the topic you are about to discuss. People with high activation might want to use this person as a second pair of ears so they don’t miss anything whereas people with lower activation might find it overwhelming to hear what you have to say.
Top tip: instead of always being physically opposite someone when you have a consultation, try walking side by side and see if they behave differently. You could do this to/from the waiting room.
Activation level support tools
There are many different ways to work out how activated a person is. Here are three tools that we have been using in Lincolnshire to support us to tailor our approaches.
Patient Activation Measure
The Flourish system. This uses 13 statements to understand behaviour and can suggest activities to increase activation through a scored process. It puts people into one of four levels.
Benefits of this approach:
- Good depth of information and supporting tools
- Tried and tested methodology
- Most detailed approach
Be careful of:
- You have to buy licences to use the PAM tool. Check out the link below for more detail
- The PAM 13, done properly, takes a bit more time than other approaches
- It requires the use of another IT system
There are Limited licences available from Insignia Health and can be purchased from the following link: Commercial License - Insignia Health
Cost are:
- Up to 500 - $2,500
- 501 – 1000 - $4,250
- 1001 – 2000 - $8,500
The pricing includes
- Patient Activation Measure® (PAM®) – All versions and translations
- Flourish – Our survey administration and scoring system that also includes a variety of self-generated reports
- Coaching for Activation® (CFA) – Our PAM-based condition support program for health coaches and providers
- Online Training and Resources – Monthly trainings, eLearning modules, PAM and CFA guides and resources
- Remote Flourish set up completed by Phreesia
For further information, you can contact naomi.dexter@phreesia.com
The 4 PAM levels look like this:
Working together
Use “we” as the partnership between you and the person that you are working with.
|
|
Strongly Agree |
Agree |
Disagree |
Strongly Disagree |
|
We know what our choices are |
|
|
|
|
|
We know how support can help us with our choices |
|
|
|
|
|
We know what is good/bad about each choice |
|
|
|
|
|
We feel ready to make a choice |
|
|
|
|
Benefits of this approach:
- Puts the focus on it being a shared responsibility
- Can support you to know what to focus on next: knowledge, support, readiness
- Helps to foster a positive relationship
Be careful of:
- Not having enough information
- Fixed mindsets. How do you know, what you don’t know?!
- Vagueness. You will need to add your specialist angle to the statements.
Ask 1 question
How would you rate your ability managing your own health and wellbeing?
1 – not able, 2 – a little able, 3 – quite able, 4 – very able.
Benefits of this approach:
- Very quick to do
- Provides a score that can be re-assessed later
- Sets the scene for further work
Be careful of:
- Causing further overwhelm by implying full responsibility is the person’s
- Not knowing what to do with the score to be able to improve knowledge, support or readiness
So what?
Perhaps you have other ways of understanding how activated a person is? Whatever method you use, tailoring your healthcare approach will help to make it more meaningful for everyone. You can even measure it using snomed codes so can show progress as people increase levels.
Time is so precious to us in a stretched service. Try to think differently about how you use it. Would some people benefit from shorter, regular appointments whereas others prefer longer more sporadic ones?
Health Coaches (and other roles) are a great resource to support people to build activation and can often get people more ready to work with specialists. Might a different intervention help get people ready to work with you?
Likewise, is there any benefit in reducing printed information for people with low activation or increasing it for those with higher activation?
After all, we know that one size doesn’t fit all!
In the above video, you can see how Amanda tailored her approaches using the Flourish approach and the benefits that gave to Hans.
Tailoring tools can improve a person’s ability to self-manage. They should be used hand in hand with approaches which include:
- health coaching – helping people gain and use the knowledge, skills and confidence to become active participants in their care so that they can reach their self-identified health and wellbeing goals
- self-management education – any form of formal education or training for people with long-term conditions focused on helping them to develop the knowledge, skills and confidence they need to manage their own health care effectively
- peer support – a range of approaches through which people with similar long-term conditions or health experiences support each other to better understand the conditions and aid recovery or self-manage
Please get in touch if you wish to discuss this further.













